Across the globe, approximately 17.5% of the adult population experiences infertility, with India reporting between 10% to 15% of married couples facing similar challenges. Among women, low AMH has emerged as one of the leading causes of difficulty in conceiving naturally, often pushing individuals to explore assisted reproductive technologies such as Intrauterine Insemination (IUI).
Dr. Hrishikesh Pai, a distinguished IVF doctor in Mumbai, emphasizes:
“Low AMH can understandably cause concern among women trying to conceive, but it’s not the end of the road. The key is timely intervention, informed decision-making, and choosing the right fertility strategy. IUI can be an effective first-line treatment in specific low AMH cases, depending on individual factors.”
So, what does low AMH mean for IUI success, and how can one improve the odds? Let’s take a deeper look into how IUI and low AMH interact.
Understanding IUI and Low AMH
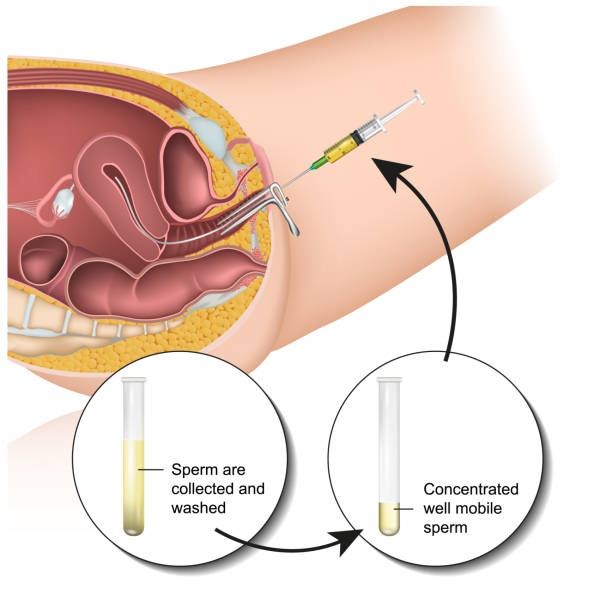
Intrauterine Insemination (IUI) is a fertility procedure in which washed and concentrated sperm are directly inserted into a woman’s uterus around the time of ovulation. This process boosts the chances of fertilization by placing the sperm closer to the egg.
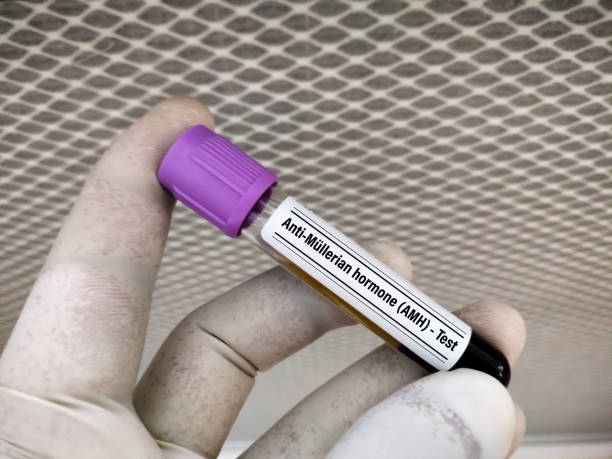
Anti-Müllerian Hormone (AMH) is a hormone secreted by follicles in the ovaries. It serves as an important marker of a woman’s ovarian reserve, or the quantity of remaining eggs. Low AMH suggests diminished egg supply, which may impact fertility outcomes.
Low AMH and fertility treatments go hand in hand. While it may limit some options, IUI remains a viable consideration under the right conditions. The success largely depends on age, egg quality, overall reproductive health, and the cause of low AMH.
Still wondering if IUI is even a possibility for women with low AMH?
Is IUI Suitable for Low AMH?
The suitability of IUI treatment for low AMH varies from person to person. Factors like age, egg quality, and male partner’s sperm health play a critical role in determining the outcome.
In general:
- Women under 35 with mild AMH decline may still benefit from IUI.
- Severely low AMH and/or age above 38 may reduce IUI success and warrant IVF.
Dr. Hrishikesh Pai, a prominent Infertility Specialist in Mumbai, shares:
“Typically, AMH levels below 1.0 ng/mL are considered low. For IUI, a level above 1.0 ng/mL is preferable, but treatment decisions should also consider age and ovarian responsiveness. Some women with borderline AMH can still benefit from IUI if their antral follicle count and hormone levels are favorable.”
In essence, AMH levels for IUI aren’t a rigid rule, but a guideline within a broader fertility profile.
Benefits of IUI with Low AMH
Despite its limitations, IUI offers several notable advantages for women with low AMH, particularly in certain age brackets and clinical situations.
Here are the potential benefits:
Less Invasive and More Affordable
Compared to IVF, IUI is less complex, less invasive, and easier on the wallet, making it an appealing first step.
Time-Sensitive Option
For younger women with reduced AMH, acting swiftly with IUI may optimize chances before ovarian reserve declines further.
Cycle Monitoring Advantage
IUI cycles involve careful monitoring of ovulation, which helps time the insemination optimally for egg release.
Natural Hormonal Stimulation
IUI can be performed in natural or mildly stimulated cycles, which is helpful for women who respond poorly to strong medications.
Emotional Ease
For some couples, starting with IUI is emotionally less overwhelming than jumping directly into IVF.
While the benefits are reassuring, it’s also important to be aware of the possible challenges associated with this route.
Potential Risks of IUI with Low AMH
Choosing IUI when you have low AMH isn’t without its share of concerns. Understanding the risks involved can help manage expectations and prepare better.
Here are key considerations:
Lower Success Rates: Women with AMH below 1.0 ng/mL have significantly lower IUI success rates compared to those with higher reserves.
Cycle Cancellations: Poor ovarian response may result in fewer or no mature follicles, leading to canceled cycles.
Emotional Impact: Multiple failed cycles can be emotionally taxing, particularly when time is a critical factor.
Limited Time Window: Low AMH typically indicates a faster decline in fertility, so relying solely on IUI may reduce the chances of overall conception success if not evaluated properly.
Dr. Hrishikesh Pai, a renowned reproductive endocrinologist in Mumbai, advises:
“Time is an important factor with low AMH. If IUI is not successful within 2–3 cycles, it may be prudent to escalate to IVF without delay. The goal should be to act swiftly and strategically to preserve chances of success.”
Ready to proceed with IUI? Here’s what the road ahead typically looks like.
What to Expect After Choosing IUI with Low AMH

After choosing Intrauterine Insemination with low AMH, you can expect a structured approach with close monitoring and hormone support. Here’s a general outline of what follows:
Ovarian Monitoring: Regular ultrasounds and blood tests will track follicle growth and hormone levels.
Ovulation Induction: Medications may be used to stimulate egg release. Timing is critical for insemination.
Sperm Preparation and Insemination: The semen sample is washed to concentrate healthy sperm, which is then inserted into the uterus during ovulation.
Luteal Phase Support: Progesterone may be prescribed to support the uterine lining post-procedure.
Dr. Pai discusses about the success rates of IUI with low AMH, “The IUI success with low AMH can vary. Women under 35 with AMH between 1.0–1.5 ng/mL may have success rates of 10–12% per cycle. For AMH <1.0 ng/mL, the success rate may drop to 5–7% per cycle. Though modest, these figures highlight that IUI isn’t entirely off the table for those with low AMH—especially if pursued early.”
But what if IUI doesn’t yield the results you’re hoping for? Let’s explore other fertility solutions.
Other Options to Consider
If IUI does not succeed or your AMH levels are severely low, alternative fertility treatments may offer better outcomes.
Here are a few options:
IVF (In Vitro Fertilization)
IVF is often more effective for women with low AMH, especially when combined with tailored stimulation protocols.
Mini-IVF
Uses lower doses of hormones to retrieve fewer but high-quality eggs. Suitable for women with poor ovarian response.
Donor Egg IVF
When ovarian reserve is too low for success with own eggs, donor eggs offer a promising path to parenthood.
Embryo Freezing (at Younger Age)
For women diagnosed early with low AMH, freezing embryos can preserve fertility for the future.
Dr. Hrishikesh Pai, often called the best IVF doctor in India, explains:
“Women with significantly low AMH may respond poorly to standard treatments. However, modern protocols, like dual stimulation or using donor gametes, can help achieve successful pregnancies even in difficult scenarios. Fertility care today is highly individualized.”
Before we wrap up, here are answers to a few questions that often come up.
Frequently Asked Questions
Can I improve AMH levels for IUI through lifestyle changes?
How many IUI cycles should be attempted with low AMH?
Does inadequate AMH indicate poor egg quality?
Are there supplements to boost AMH before IUI?
Can low AMH cause miscarriage after IUI?
References:
https://rmanetwork.com/blog/anti-mullerian-hormone-amh-testing-of-ovarian-reserve/
https://my.clevelandclinic.org/health/diagnostics/22681-anti-mullerian-hormone-test
Disclaimer: The information shared in this content is for educational purposes only and not for promotional use.

